The traveling exhibit “Native Voices: Native Peoples’ Concepts of Health and Illness” opens June 9 in Anchorage.
RELATED: 9 Great Places to Experience American and Native Culture
Starting at the Dena’ina Center, the exhibit will debut with a noon luncheon ceremony featuring the Southcentral Foundation, the Alaska Native Heritage Center and the National Congress of American Indians.
The exhibit will remain open for visitors of the Conference of the National Congress of American Indians until June 12, and then it will open to the general public at the Alaska Native Heritage Center from June 13 through mid-September.
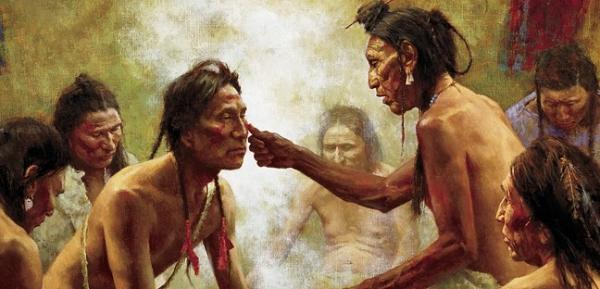
Oral history and the wisdom of medicine men are recognized in the traveling exhibit, which made its grand debut at the National Institutes of Health’s National Library of Medicine in Bethesda, Maryland with a blessing ceremony on October 5, 2011.
Some of the most revered native healers were interviewed for the project, plus tribal educators, curators and others. “One of the major goals is to share from the native community and in their own words and own descriptions what is important to them in terms of native concepts of health, healing and illness,” Fred Wood, a National Library of Medicine curator involved with the project’s development, said. “We’re doing our best to make that in their words, not someone else’s interpretation.”
RELATED: The Lummi Healing Totem Pole Carries Stories of Traditional Medicines and Practices
Topics featured in the exhibition include: Native views of land, food, community, Earth/nature, and spirituality as they relate to Native health; the relationship between traditional healing and Western medicine in Native communities; economic and cultural issues that affect the health of Native communities; efforts by Native communities to improve health conditions; and the role of Native Americans in military service and healing support for returning Native veterans.
Indian Health Service Director, Dr. Yvette Roubideaux, a featured speaker at the opening ceremony, said the concept for the exhibition grew out of meetings with Native leaders throughout the nation, “and reflects the Native tradition of oral history… This wonderful exhibit is helping to make Native voices and cultural perspectives seen and heard, and to promote understanding and appreciation of Native cultures.”
For web browsers all over the world, photos and summaries on the web site pull out specific aspects of the exhibit, such as the healing properties of certain plants. The introduction to the “Medicine Ways” section states that “[m]any traditional healers say that most of the healing is done by the patient and that every person has a responsibility for his or her proper behavior and health. This is a serious, lifelong responsibility. Healers serve as facilitators and counselors to help patients heal themselves. Healers use stories, humor, music, tobacco, smudging, and ceremonies to bring healing energies into the healing space and focus their effects.”
Ceremonial drums, pipes and rattles from Upper Plains tribes are displayed in one section on healing. Another explores ceremonies that traditional healers performed to give relief to returning veterans who suffered from combat-related stress. “Because physical and spiritual health are intimately connected, body and spirit must heal together,” says printed material in the exhibit, on “The Key Role of Ceremony.”
Another section explores Native games “for survival, strength and sports.” Surfing figures big here, as the exhibit pays tribute to Duke Kahanamoku, Native Hawaiian Olympic medallist who is credited with reviving surfboarding as a sport. In the lobby of the library is a 10-foot model of the Hokule‘a, a traditional Hawaiian voyaging canoe. It is intended to show visitors “how the mission of the Hokule‘a has spurred a Hawaiian cultural and health revival.”
Read more at http://indiancountrytodaymedianetwork.com/2014/06/09/traveling-native-voices-health-exhibit-opens-today-anchorage-155212?page=0%2C1