Category: Health
Indian Country Grapples With Health Funding Shortfalls, Non-Payment
Slowly but surely, tribal governments — especially those in Alaska — are receiving millions of dollars in decades of unpaid contract costs from the Indian Health Service and Bureau of Indian Affairs.

WASHINGTON — Tribal health programs working to serve native people are not seeing funding of administrative costs keeping pace with need, and the Indian Health Service and the Bureau of Indian Affairs owe millions to tribal governments.
“The federal government has broken too many promises with tribes and though we have more work to do, I am pleased that we are seeing good progress with Alaska tribes receiving the money they are owed,” Alaska Sen. Mark Begich told the Alaska Native Tribal Health Consortium last month. “Failure to pay the full costs is unacceptable and I will continue to use my position on the Senate Indian Affairs Committee to keep up the pressure on the federal government.”
The IHS, a Department of Health and Human Services agency, provides health service systems for about 2.2 million of the nation’s estimated 3.4 million American Indians and Alaska Natives.
Funds allocated by the IHS, currently $4.4 billion per year, go toward administering medical care to tribes or are turned over to tribes for them to administer the care themselves. The IHS had been failing to provide full payments of contract costs until the Supreme Court ruled in June 2012 that the government must pay, determining that the tribes had been underpaid “between 77 percent and 92 percent of the tribes’ aggregate contract support costs” during previous decades.
Yet, according to Jacqueline Johnson Pata, executive director of the National Congress of American Indians, “payment has not happened.”
“The class action lawyers recently reported to NCAI on the lawyer’s discussions with the Justice Department. Although they couldn’t share much information, they did explain that there are close to 9,000 claim years at issue involving about 500 tribes and 19 years worth of contracts (1994-2013),” she told the U.S. Senate Committee of Indian Affairs last year.
Sen. Begich introduced Senate Bill 2669 in July to the Senate Appropriations Committee
to mandate funding for certain payments to Indian tribes and tribal organization. Additionally, the federal government has treaty and statutory obligations under the Indian Self-Determination and Education Assistance Act of 1975, which requires the government to contract with tribes to operate BIA and IHS programs. The agreement between the government and tribes is embedded in Article I, Section 8, of the U.S. Constitution.
At the end of 2013, less than 1 percent of thousands of claims in more than 200 lawsuits filed by tribes seeking a combined $200 billion had been settled — just 16 claims of an estimated 1,600.
Of the 566 nations the federal government recognizes, 229 are spread across the vast 572,000 square miles of Alaska, where they occupy small villages in remote areas — many only accessible by air or boat. For these tribes in remote areas, seeing a doctor might be inconvenient, to say the least, and almost definitely costly.
Lead counsel in the cases establishing government liability for IHS’s failure to pay, Lloyd Miller, an attorney based in Anchorage, Alaska, said IHS is severely underfunded.
“IHS is a prepared health plan paid for with a lot of blood and millions of acres of land,” Miller said. “Because the government took away their lands, there’s a responsibility.”
IHS gets $4.4 billion from Congress annually for what’s estimated to be a $15 billion need to meet the costs, he said.
Miller represents about 60 tribes, each with several claims filed for the costs owed.
In an August 2007 letter to the Senate Committee on Indian Affairs requesting an oversight hearing, Alaskan tribal health care providers reminded the committee that the Indian Self-Determination Act requires money to provide federal trust responsibilities.
“We write to once again call your attention to the grave crisis we face as a result of insufficient contract support cost appropriations which, together with Indian Health Service policies, have left our tribal organizations with annual shortfalls running from $2 million to over $8 million. We respectfully request that the Senate Indian Affairs Committee convene an urgent oversight hearing this Fall, to review what has become a genuine crisis in Indian country, and a crisis that has seriously eroded the national policy of Tribal self-governance and the delivery of quality health services to Alaska Native people,” the letter stated.
By August of this year, 12 of Alaska’s tribal health providers received $449 million to resolve contract support costs disputes with the IHS. Another 11 providers were still in negotiations. The Alaska Native Tribal Health Consortium, serving more than 143,000 native people, received the largest payment, with a $153 million settlement that includes $115.5 for past-due costs and $37.7 million in interest. At about $128 million, Southcentral Foundation received the next largest settlement.
The NCAI has been working with tribes and the IHS on contract costs since the Indian Self-Determination Act went into effect.
The congress is hosting the annual Tribal Unity Gathering and Legislative Impact Days on Sept. 16 and 17 in Washington. During the event, tribal leaders and representatives will meet with their delegates to the U.S. Congress to encourage action on important delegation before this session ends. IHS appropriations will be among the issues discussed.
“There’s strong support from the House and Senate,” said Amber Eberb, program manager of the NCAI Policy Research Center. “There’s quite a few champions who understand that tribes administering their own programs to respond to their community needs is more effective than a federal agency.”
There’s still progress to be made, Eberb said.
“Contract costs and other treaty issues should not be considered discretionary but mandatory,” Ebarb said. “All program money that uphold treaty agreements should be mandatory. It’s morally correct to do. Perhaps a little difficult to do right now.”
Disparities in well-being
American Indian and Alaska Native (AI/AN) death rates were nearly 50 percent greater than rates among non-Hispanic whites during 1999-2009, according to a study by the Centers for Disease Control.
The study was carried out by the CDC’s Division of Cancer Prevention and Control, the CDC’s National Center for Health Statistics, CDC researchers, the IHS, and partners from tribal groups, universities and state health departments.
It revealed:
Among AI/AN people, cancer is the leading cause of death, followed by heart disease, while the opposite is true for other races studied;
- Death rates from lung cancer have shown little improvement in AI/AN populations. AI/AN people have the highest prevalence of tobacco use of any population in the United States;
- Deaths from injuries were higher among AI/AN people compared to non-Hispanic whites;
- Suicide rates were nearly 50 percent higher for AI/AN people compared to non-Hispanic whites, and more frequent among AI/AN males and persons under age 25;
- Death rates from motor vehicle crashes, poisoning, and falls were two times higher among AI/AN people than for non-Hispanic whites;
- Death rates were higher among AI/AN infants compared to non-Hispanic white infants. Sudden infant death syndrome and unintentional injuries were also more common. AI/AN infants were four times more likely to die from pneumonia and influenza;
- By region, the highest mortality rates were in the Northern Plains and Southern Plains, while the East and Southwest had the lowest.
“Many of the observed excess deaths can be addressed through evidence-based public health interventions,” the report concluded.
In November 2013 testimony before the Senate Committee on Indian Affairs, Alaska Sen. Lisa Murkowski said:
“I listened very intently yesterday at the tribal summit when the President spoke. I went there specifically to hear what he was going to say on the issue of contract support costs. What I heard him say is, we have heard you loud and clear, but we are still working to find the answers. I don’t think we need to work to find any answers. I think that the court laid it out very, very clearly. It said that full reimbursement will be provided. So we have to make that happen within that budget. We have to make that priority.”
Murkowski said she had listened to the stories of the impact of lack of funds, saying, for example, that the regional health provider in Juneau had to close its alcohol treatment facility. Further north, in the Yukon Delta, the regional health provider laid off 20 employees, permanently closed 40 vacant positions, and reduced services for elders, she continued.
The impacts of the sequestration, she said, also meant that tribes would not be able to reduce waiting times at emergency rooms or outpatient and dental clinics.
“The impact, I think we recognize, has been significant,” she said.
Murkowski submitted comments she received from Alaska Natives around the state, including the Association of Village Council Presidents.
Proposed Increase for IHS Budget
“Tribes have not recovered from sequestration that resulted in across-the-board cuts to all federal programs that tribes are reliant upon. Nowhere was this more impactful than to the Indian Health Services, where due to sequestration, continuing resolutions, and the 16 day government shutdown — healthcare to Indian people was jeopardized,” U.S. Senate Committee on Indian Affairs Chairman Jon Tester, of Montana, said in March.
Tami Truette Jerue, tribal administrator and director of social services for the Anvik Tribal Council in Alaska addressed the committee’s oversight hearing in February. The Anvik are an Athabascan village of about 275 members on the west bank of the Yukon River.
Jerue represented the 37 federally recognized tribes that make up the Tanana Chiefs Conference, an inter-tribal health and social services consortium that serves an area of Interior Alaska that is roughly the size of Texas.
She delivered a message from more than 200 tribes across Alaska:
“It is absolutely essential that, without regard to technical land titles and the technical Indian country status of lands or tribal communities, our Tribes must have the tools necessary to combat drug and alcohol abuse, domestic violence, and violence against women. Fighting these scourges in our communities and healing our people cannot be made to stand on technicalities. We need to get to work, and now. And we need Congress’s help to do that. The State is not the problem, because the State is nowhere to be found in most of our Villages….
“Today, the tribes of Alaska come to you, not as victims of a failed governmental policy, but as powerful and responsible advocates for our people. We are stepping up to do what we must do. But without equally firm action from Congress, our people will suffer, we will continue with decades more of litigation battles and loopholes will continue to be found which deny our tribes the funding necessary to improve law and order in our communities.”
In the budget for the 2015 fiscal year, the Obama administration proposed a 4.5 percent increase for IHS, representing a $200 million increase over the current level to $4.6 billion.
The 2015 budget request includes:
- An additional $50 million to help obtain health care from the private sector through the Purchased/Referred Care program (formerly known as the Contract Health Services program). This program allows for the purchase of essential health care services that the IHS and tribes do not provide in their local facilities;
- An additional $71 million to support staffing and operating costs at four new and expanded facilities;
- An additional $30 million to fully fund the estimated amount of contract support costs for new and expanded contracts and compacts in fiscal year 2015. This will help tribes cover the cost of administrative functions for compacts or contracts established under the authority of the Indian Self-Determination and Education Assistance Act;
- An additional $31 million to address medical inflation costs;
- Additional funding to pay costs for new tribes and restoration of reductions in the fiscal year 2014 operating plan.
In his statement, Tester noted the “positive highlights” in the budget request.
“The Committee is pleased that the Administration finally understands its legal obligation to fully fund Contract Support Costs for the both the Indian Health Service and Bureau of Indian Affairs,” Tester said. “I am particularly encouraged by the $11 million increase for social services and job training to support an initiative to provide a comprehensive and integrated approach to address the problems of violence, poverty, and substance abuse.”
Covering IHS shortfalls with the Affordable Care Act
The Southeast Alaska Regional Health Consortium and more than 50 tribes wrote a letter to President Obama on Oct. 13.
In part, it said, “Among your administration’s most important achievements has been the development of historic settlements with Indian Tribes in several major litigations, its advocacy for amendments to the Indian Health Care Improvement Act and the Violence Against Women’s Act, and its commitment to critical appropriations measures. But when it comes to honoring the Nation’s commitment to the contracting and compacting Tribes who were historically, and illegally, underpaid, and who continue to be underpaid, the administration has permitted fiscal concerns to eclipse the imperative to do justice and to honor the nation’s obligations.”
In July the IHS reached a settlement with the consortium for claims during the years 1999 through 2013. The payment — $39.5 million plus interest — totals about $53 million.
“A lot of tribes had to close down programs because of lack of funds,” Andrea Thomas, outreach and enrollment manager of SEARHC, told MintPress News. “Part of what the settlement can do is bring back what was lost.”
Alaska did not create reservations like the 48 contiguous states, and many Native communities formed consortiums, like SEARHC, to use IHS funding for health care to serve them all.
SEARHC is a nonprofit tribal health consortium of 18 Native communities which serves the health interests of the Tlingit, Haida, Tsimshian, and other Native people of Southeast Alaska. In 1982, the consortium took over operations at the IHS clinic in Juneau, and then took over operations at Mt. Edgecumbe Hospital, formerly an IHS-run facility, in 1986.
“In Alaska we have the highest cost of health care in the nation,” Thomas said. “There’s vast wilderness surrounding each place. In order for me to get out of my community, I’d have to fly or take a ferry. This gets incredibly expensive.”
Many Alaskan villages have a community health clinic, but complicated procedures such as chemotherapy or serious surgeries, require patients to go to hospitals at regional hubs or to the Alaska Native Medical Center in Anchorage. The burden is on the tribal health consortium to pay the costs of a commercial jet, float plane, ferry, or boat.
If a medical evacuation helicopter is needed, it would cost SEARHC about $95,000 — a cost that could be absorbed by the Affordable Care Act.
“The issue is that IHS only provides about half the money for services,” Thomas said. “We rely on other revenues like grants and billing Medicare and Medicaid. If native people enroll, it puts more money back and we could offer more services or expanded services.”
Further, a member of a federally recognized tribe can get a lifetime exemption. Alaska Natives and American Indians are exempt from Affordable Care Act tax penalties because they receive care through the IHS. But through the new health care scheme, they are eligible for subsidies from private insurance. Thomas said that those who fall between 100 percent and 500 percent of the federal poverty level pay a monthly premium, but no deductibles or out-of-pocket expenses.
Yet, of more than 100,000 self-identified Alaskan Natives or American Indians, only 115 had signed up for health insurance through the Affordable Care Act as of April.
“Not a lot of people realize what the Affordable Care Act does for Alaskan Native people,” Thomas said.
Coverage also extends to Native people who are not enrolled members of a federally recognized tribe and meet federal guidelines. Thomas said they can receive a lifetime hardship exemption, rather than a tribal exemption, and there may be some out-of-pocket expense.
Shellfish Tell Puget Sound’s Polluted Tale
By Ashley Ahearn, KUOW

SEATTLE — Scientists used shellfish to conduct the broadest study to date of pollution levels along the shore of Puget Sound.
And in some places, it’s pretty contaminated.
This past winter the Washington Department of Fish and Wildlife put mussels at more than 100 sites up and down Puget Sound.
After a few months, volunteers and WDFW employees gathered the shellfish and analyzed them for metals, fossil fuel pollution, flame-retardants and other chemicals. The WDFW just released the results.
“The biggest concentrations of those contaminants were found in the highly urbanized bays – Elliott Bay, Salmon Bay, in the Sinclair Inlet, Commencement Bay we found much higher contaminations than we did in the rest of Puget Sound,” said Jennifer Lanksbury, a biologist who led the study for the Department of Fish and Wildlife.
PAHs – or polycyclic aromatic hydrocarbons – were found in mussels at every single test site. PAHs come from fossil fuels – spilled oil, wood stove smoke and engine exhaust, mainly. The particles can be deposited through the air or get washed into Puget Sound when it rains. Some PAHs are carcinogenic.
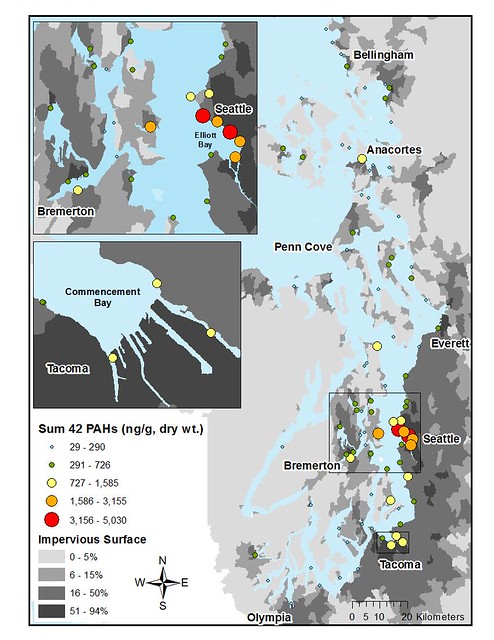
Map of PAH levels in Puget Sound. Credit: WDFW
The mussel samples all contained PCBs as well. Flame retardants and DDT were found at more than 90 percent of the sites – with the highest levels in more urban bays.
“This is showing that these contaminants are entering the nearshore food web and they’re likely being passed up to other higher organisms and people eat mussels too,” Lanksbury added.
The state Department of Health does rigorous testing for toxic algae and bacteria in shellfish – the kind of stuff that makes you sick immediately. But it doesn’t regularly test shellfish for metals and other contaminants that can harm human health over longer periods of exposure.
“PAH is a difficult issue,” said Dave McBride with the Department of Health. “They are widespread in the environment. We probably get a lot greater exposure to PAHs from the food we eat on the grill, hamburgers or smoked salmon. It’s all relative. Some of the PAHs are considered carcinogens so it’s definitely on our radar.”
Shellfish harvest, in general, is limited in dense urban areas – where the DFW’s mussel study showed the highest levels of contaminants. However, this past winter China banned all imports of shellfish from much of the west coast after finding elevated levels of arsenic in some shellfish harvested near Tacoma.

Volunteers Jonathan Frodge, Chris Wilke and Paul
Fredrickson gather mussel samples at Discovery
Park in Seattle. Credit: Tom Foley
Lanksbury says that she still feels safe eating mussels and other shellfish from Puget Sound. And, she adds, there are things people can do to lower pollution levels.
“When they say, don’t let your car drip oil, support low-impact development where they’re having rain gardens, don’t wash your car on the side of the road – all of those kinds of things spare Puget Sound from contaminants that we produce on a daily basis by burning fossil fuels,” Lanksbury said.
The Department of Fish and Wildlife hopes to keep the mussel monitoring program going, with the continued help of more than 100 volunteers and citizen scientists from around Puget Sound.
Flu Season 2014-2015 – Public Service Announcement from the Karen I. Fryberg Tulalip Health Clinic
Fewer hungry humans — but still too many

By Nathanael Johnson, Grist
Which country has the highest percentage of hungry people? I’ll put the answer at the bottom. (Hint: it’s not located in Africa.)
The United Nations’ annual report on hunger has arrived bearing sobering factoids like this one, along with some remarkably good news: There are now 100 million fewer chronically hungry people than there were 10 years ago.
The improvements vary dramatically. In southeast Asia, 30 percent of people were undernourished in 1992; now it’s down to 10 percent, a stunning accomplishment. But in the Middle East (here labeled western Asia), the percentage of undernourished people has actually gone up. Worldwide, 11 percent of people still go through most of their lives hungry.

The UN’s Food and Agriculture Organization says that the Millennium Development Goals on hunger are within reach “if appropriate and immediate efforts are stepped up.”
What form should those efforts take? The UN urges everyone to remember that hunger is a fundamentally political problem:
Lack of food, as we’ve said, is not the problem. The world produces enough food for everyone to be properly nourished and lead a healthy and productive life. Hunger exists because of poverty, natural disasters, earthquakes, floods and droughts. Women are particularly affected. In many countries they do most of the farming, but do not have the same access as men to training, credit or land.
Hunger exists because of conflict and war, which destroy the chance to earn a decent living. It exists because poor people don’t have access to land to grow viable crops or keep livestock, or to steady work that would give them an income to buy food. It exists because people sometimes use natural resources in ways that are not sustainable. It exists because there is not enough investment in the rural sector in many countries to support agricultural development. Hunger exists because financial and economic crises affect the poor most of all by reducing or eliminating the sources of income they depend on to survive.
And finally it exists because there is not yet the political will and commitment to make the changes needed to end hunger, once and for all.
But how do you go about fixing those problems and mustering the political will? The new report suggests:
Hunger reduction requires an integrated approach, which would include: public and private investments to raise agricultural productivity; better access to inputs, land, services, technologies and markets; measures to promote rural development; social protection for the most vulnerable, including strengthening their resilience to conflicts and natural disasters; and specific nutrition programmes, especially to address micronutrient deficiencies in mothers and children under five.
In other words, the technical solutions can help with the political solutions and vice versa. This is a bit of a chicken and egg problem: Which do you do first: stop the war, or help farmers grow more food? If people are hungry, perhaps it’s better to send grain rather than soldiers. But if militants grab and sell the grain, we’re back to square one. The answer to the chicken and egg question seems to be: both.
As for the answer to the question I began with: Haiti is the nation with the highest percentage of hungry citizens. An astonishing 52 percent of people there are undernourished.
Scientists On A Quest For Knowledge About Coal Dust Risks
By Ashley Ahearn, KUOW
WASHOUGAL, Wash. — Coal had been transported around the country by rail for decades before the recent push to bring it by train to ports in the Northwest.
And yet, scientists don’t really know how much coal dust could escape from rail cars, how far it might travel, and what coal-borne mercury and other contaminants might do to aquatic life.
With the permitting process moving forward for two large coal terminals in Washington, a team of scientists with the U.S. Geological Survey is trying to find out how the chemicals in coal might interact with the environment.
“We really don’t know what the effects are and whether it is an issue,” says Bob Black, a scientist with the USGS.
Black is the lead scientist on the new study, which has him squelching through the muck at the Steigerwald Wildlife Refuge near Washougal, Washington. The refuge is sandwiched between the Columbia River to the south, and train tracks to the north.
Black and his team are gathering data for a first-of-its kind scientific study of coal and its potential impacts on wetland ecosystems. As he sloshes through the shallow marsh’s waters to plant minnow traps, Black says he knows that he’s also wading into a controversial issue.
“There are communities that are economically interested in this and then there are suggested environmental impacts and ultimately I can have my own personal views but I can’t let those come into play and essentially that’s our role. We can’t let that be part of our science,” Black says.
The team fans out across the marsh as a BNSF Railway train screeches along tracks less than a quarter-mile away. This train is not hauling coal. Right now, roughly one coal train per day travels along the Columbia River before turning north and following the shoreline of Puget Sound to service Canadian coal terminals. But if terminals are built in Longview and near Bellingham, that number could jump to more than 20 coal trains per day.
Some coal does escape from trains, as BNSF has testified publicly in the past. Environmental groups have sued BNSF Railway for violating the Clean Water Act by allowing coal and coal dust to escape from trains and get into waterways along tracks in the Northwest. A judge ruled this month in favor of local groups in Seward, Alaska after they sued a nearby coal terminal for similar Clean Water Act violations. However, supporters of coal exports have called the coal escapement issue a red herring, used by anti-coal environmental groups to spark public alarm.
Looking For Coal Clues
The USGS is gathering samples of muck, fish and insects from two sites in this wildlife refuge, one close to the tracks, the other farther away. The goal is to find out whether more mercury and polycyclic aromatic hydrocarbons (PAHs) are showing up near the train tracks and how those contaminants are behaving in the environment.

Collin Eagles-Smith hunts for dragonfly larvae at Stiegerwald
Lake National Wildlife Refuge. Credit: Ashley Ahearn
Collin Eagles-Smith, an ecologist with USGS, stands thigh-deep in the marsh, net in hand. He’s sifting through handfuls of black muck, looking for dragonfly larvae. When he finds one, he opens his palm to display the specimen before putting it in a little plastic baggy to take back to the lab for analysis. Eagles-Smith says dragonflies can serve as vectors to transmit mercury contamination out of the aquatic environment and into land-based ecosystems because they feed on all kinds of plankton and other tiny organisms. When they grow up and fly out of the muck they are in turn eaten by birds, frogs, fish and other animals, potentially transferring mercury contamination up the food chain.
“So what we’re looking at is essentially, is there mercury in this dragonfly and then we’re going to be using a fairly sophisticated approach to fingerprint the isotope ratios of the mercury to see if we can say whether the mercury in this dragonfly was from coal dust,” he explains.
By comparing dragonfly larvae, sediment and fish samples from this site with those from another site farther from the tracks, the team hopes to see how far contamination from coal trains could travel. But Eagles-Smith says there are still a lot of questions about how active the mercury in coal might be if it gets into the environment. Mercury is believed to be inert and less harmful to the environment until it goes through a complex biological process known as mercury methylation.
“I like to think of it as activating the mercury, and it makes it more biologically available, more toxic. Do you smell that rotten egg smell?” Eagles-Smith asks from his mucky perch. “That is the smell of tiny organisms breaking down organic material. Those same organisms are the ones that take the mercury, the less toxic form of mercury, and convert it into the methyl mercury.”
Once it’s methylated, mercury has been shown to be a potent neurotoxin, Eagles-Smith explains. “It can influence stress hormones, thyroid hormones, and sex hormones so it can impact wildlife reproduction, fish behavior, their survival, their ability to hunt for prey or their ability to avoid predation.”
The unique rotten-egg decaying process that takes place in low-oxygen marshy environments like this means that wetlands could be hotspots for transforming inert mercury from coal into a more toxic and biologically-available form that can then make its way up the food chain, the scientists worry.
Emerging technology is helping scientists zoom in on more specific sources of mercury pollution in the environment. Mercury can travel in air pollution for thousands of miles. But scientists want to know if coal trains that pass through wetlands like this might serve as a sort of direct deposit of mercury pollution.
The USGS expects to have preliminary results within the next 6 months, though the researchers caution that this is a small sample size and more study is needed. The results will be shared with the state and federal agencies that are studying the environmental impacts of the two proposed coal terminals in the Northwest.
1st Annual Homecoming 5k fun Run/Walk
The Marysville Pilchuck Tomahawk Booster club and the Tomahawk Cross Country Team are hosting this 1st Annual Homecoming 5k fun Run/Walk.
Break out the old dance attire, you will be running to the soft rock hits of the 80s and competing for some cool prizes while getting your fitness on.
Visit mpbosters.com for online registration.
Jade Parks, finding her own beauty
A story of weight loss, self-esteem and learning who you are beyond the scale
By Brandi N. Montreuil, Tulalip News

Photo courtesy/ Jade Parks
TULALIP – On January 17, of this year, Tulalip tribal member Jade Parks was in Mexico, following a major surgery, she was 350 pounds and a dress size 26. She was alone except for her best friend and had just started a journey that would alter her life drastically to reveal a woman she never knew existed.
Growing up, Jade was always larger than her peers. Shopping in plus size stores became regular as she entered adulthood. She didn’t shy away from life despite her larger size, she learned to accommodate it instead. Yet as her weight continued to increase, her usual bubbly personality began to shrink, eventually leading to depression after years of losing and gaining weight. Something had to change.
Parks sought help from her tribal council to pay for a surgical procedure to help her lose weight. Due to a policy that required her to be experiencing two major health issues as a result of her weight, she was denied. She weighed over 300 pounds and suffered high blood pressure and sleep apnea. These did not qualify.
Despite being denied the monetary help, Parks was determined to lose weight. Through diet, exercise and enrollment as an outpatient in treatment for food addiction, Parks lost 73 pounds in 9 months. But it didn’t last. Parks eventually gained back the pounds she lost, plus seven more.
“It was extremely depressing. I was really sad and I didn’t know what I was going to do. You wake up in the morning not wanting to eat bad things, wanting to make good choices, wanting to work out and then you look in the mirror, and you just feel like a failure because of your weight. You think, how could I let myself get like this,” said Parks, about a typical day for her.
“It is hard. For plus size people, when you walk into the room everyone knows your issue. It is not something you can hide. I can’t hide my addiction. I can’t hide what my issue is, because it is the first thing you see when you see me, because it is my weight. A lot of times drug addicts can hide their substance abuse, people do not know that they abuse drugs. For us, as soon as we walk into a room, every single person is going to know and that makes it hard. It came basically down to: I can’t live like this anymore. I can’t live at being 350 pounds. I decided to pay for the weight loss surgery on my own, so I went to Mexico because it is cheaper.”
Although risks can be associated with medical treatment in other countries, Parks’ research led her to a private hospital and a surgical staff that she was comfortable with and she made plans to travel.
“I have never had surgery in my life before. I was worried about it, but I was more worried about not ever being able to have kids because of my weight,” said Parks, who developed polycystic ovary syndrome as a result of her weight, which caused her to stop menstruating.
Parks had a sleeve gastrectomy, which involves a portion of the stomach being separated and removed from the body. According to the Mayo Clinic, the “remaining section is formed into a tube-like structure. The smaller stomach cannot hold as much food. It also produces less of the appetite-regulating hormone ghrelin, which may lessen your desire to eat. However, sleeve gastrectomy does not affect absorption of calories and nutrients in the intestines.” This type of surgery, unlike other weight loss surgeries such as the gastric banding, is irreversible and still considered a relatively new procedure in America, meaning its long-term effects are still being evaluated.

Photo courtesy/ Jade Parks
“People think that weight loss surgery is the easy way out, but I am here to say that it is not an easy way out. It is extremely hard, because you still battle cravings and wanting foods. I can eat about four bites of food and I am full,” said Parks, who had 80 percent of her stomach removed during the surgery and can only take quarter sized bites while

eating.
“There are a lot of people who get weight loss surgery and abuse it. They stretch out their stomachs and gain the weight back. I have followed the diet from the doctor very strictly. For instance, you cannot eat and drink at the same time. You have to do it within half an hour of each other, and that’s because there is not enough room. If you do, it will stretch out your stomach,” explains Parks, who also cannot have carbonated beverages and will need to maintain the strict diet for the rest of her life.
Due to the diet’s strict portion control, Parks takes a regimen of vitamins to ensure she receives the proper amount of nutrients for her body, including choosing portion options that include the natural nutrients in them.
Weight loss surgery creates dramatic changes in physical appearance, causing unexpected emotional impacts in patients. These sudden changes often leave patients unprepared to cope with the lifestyle and dieting required following surgery, leading to a continuance or return to the eating habits that led to their weight gain. A majority of patients view weight loss surgery as a cure-all to their weight issues which can mislead them, resulting in unsuccessful weight loss. Patients considering weight loss surgery should consider the pros and cons related to the surgery and following it.
“You have to be careful because you are getting rid of one of your addictions,” said Parks, who was on a liquid diet the first month following her surgery. “That first month I was a wreck. I couldn’t smoke. I couldn’t workout and I couldn’t eat. Those are my vices. I did a lot of crying, a lot of sitting with my feelings and having to just deal with life. At the same time, it helped to prepare me for the rest of my weight loss journey, because I can’t continue to use food as my coping mechanism. It helped me learn to sit with my feelings and learn that feeling emotions is not going to kill you, and that you have to let yourself feel emotions.”
“My biggest fear about getting the weight loss surgery was that I would get the surgery and then I would regret it. There is nothing that I have experienced through this journey that has ever made me regret my surgery. It truly is the best decision I have made for myself,” said Parks, who has lost a total of 131 pounds at the time of this article.
Although weight loss surgery is not recommended for everyone, or may not be successful for everyone who has it, Parks explains that the nine months following her surgery has taught her more about herself than she ever expected.
“I have always known I am a strong woman, but now I truly believe it. To know that so many people get weight loss surgery and it just doesn’t work for them, it makes me feel stronger and gives me such a sense of pride to know have come this far. That I am able to follow the rules and stick to what I am supposed to and not throw up, is a huge thing. Now I don’t need a seat belt extender on an airplane. When I park really close to another car, I can squeeze out without my car door hitting the other car. I can fit into chairs. I can cross my legs. I have had to move my seat up in my car. I have been able to shop in non-plus size stores. Normal jewelry fits me,” said Parks about the little things she enjoys about her weight loss.

Photo courtesy/ Jade Parks
“You really have to know that this is something that you want and you are willing to make the sacrifices it takes to get it done, and do it the right way. A lot of people think they are ready because they are just tired of being big for so long, but it is a hard road. It is a good idea to be in therapy or something to help you through the journey, because when you can no longer use food as your coping mechanism, you need to be able to work through your emotions and whatever life is throwing at you. In the end it is worth it. I wouldn’t take it back for anything,” said Parks, who plans to continue her doctors’ diet plan, working out and living a healthier life.
“I am never going back to 350 pounds. I am never going to go back to a size 26. I am never going back to using food as a way to deal with life.”
Marine Survival Project Looks at Salmon Poisoning Disease
Source: Northwest Indian Fisheries Commission
Steelhead out-migrating from North Sound rivers appear to have better marine survival than steelhead smolts from South Sound, and researchers are studying salmon poisoning disease as a potential cause.
Salmon poisoning disease, or Nanophyetus salmincola, is best known as the parasite that can make dogs sick when they eat raw salmon. It also has been found to affect the swimming performance of infected salmonids, potentially reducing their marine survival.
Fish pathologist Martin Chen is studying steelhead smolts for the NWIFC as part of the Salish Sea Marine Survival Project. Chen is sampling steelhead from the Tahuya, Skagit, Snohomish, Green and Nisqually rivers.
“We thought Skagit and Snohomish would be negative for the parasite based on historical records, and that was true,” Chen said. “We found lots of heavily infected fish in the Green and Nisqually rivers. I can see the parasite even as I’m dissecting them. Parasite numbers are as high as 18,000 per gram of kidney tissue.”
Both of those results were expected, but Chen was surprised not to find the parasite in any of the 24 steelhead sampled from the Tahuya River in Hood Canal. The Tahuya is across the canal from the Skokomish River, which has Nanophyetus in at least three tributaries.
South Sound fish also have their marine survival challenged by swimming through the Tacoma Narrows and Point Defiance, and facing more predation from seals. To make a more even comparison, researchers placed infected South Sound fish and uninfected North Sound fish in the same saltwater environment to compare survival. After 90 days in saltwater tanks at the USGS Marrowstone Island Laboratory, both groups had the same high survival rate.
“The fish from the Green River are still heavily infected,” Chen said. “It’s possible that infected fish have some disadvantage and they’re less able to escape predators. They don’t just hit the salt water and roll over and die.”
Chen also is testing drugs that could eliminate the parasite from infected fish. Two drugs are being tested on small numbers of coho at the Nisqually Tribe’s Clear Creek Hatchery, with some coho getting a 24-hour bath of each drug, and other fish having a drug mixed in their food. None of the fish from this initial test will be released or eaten.
“If the drugs were effective and you were rearing fish in a parasite-positive environment, you could clean up a group of fish before releasing them,” Chen said. “You would no longer have to compare survival of fish between two river systems, making our studies more valid. In addition, being able to eliminate Nanophyetus before release could have a practical application for Northwest hatcheries.”
Alaska Natives Wait… And Wait, For Health Law Exemption
Most Americans are supposed to have health insurance under the Affordable Care Act. But up to 50,000 Alaska Natives and American Indians in Alaska are excused from the requirement. They have to apply for that lifetime exemption though. And the federal government is mishandling many of those applications.
By Annie Feidt, Alaska Public Media Network
Evelyn Burdick thought it would be easy to apply for her American Indian exemption. As a member of the Cherokee Nation, the Anchorage resident sees a doctor at the Alaska Native Medical Center. Burdick likes the care she gets there and has no plans to sign up for private insurance under Obamacare. So she sent an exemption application to the federal government almost as soon as it was available, on January 9th:
“I have yet to receive any correspondence from them back whatsoever. Not even to let me know they’ve received my application.”
Burdick is not alone. The Alaska Native Tribal Health Consortium has helped hundreds of Alaska Natives and American Indians in the state who have had problems with their exemption applications. The exemption is a simple six digit number applicants need for their tax forms to avoid paying a penalty ($95 dollars or 1% of income, whichever is greater) for not having health insurance. Monique Martin, with ANTHC, has been working with the federal government to resolve the problems:
“Every time we call it’s a bear with us sort of request but we’ve been bearing with them since February when we first started reporting issues and we are anxious for a resolution to this issue.”
The Federal government has fumbled the applications in several different ways. Martin works closely with three other people at ANTHC who all applied for the exemption for themselves. Martin’s exemption number came back with no problems. But her three colleagues were not so lucky:
“One of our coworkers received her letter twice, with two different exemption numbers for her and her kids. One received the wrong exemption… and another one is still waiting to hear on her application. So we’ve seen all the errors come to us, so we have real world examples that we can show the federal government.”
No one from the Centers for Medicare and Medicaid Services was willing to do an interview for this story. In an e-mail, a spokesperson with the agency wrote that they are working to improve the process daily and committed to providing consumers with their exemption numbers in time for tax filing season. Martin says she’s cautiously optimistic that can happen:
“We are the squeaky wheel in Alaska and we’re really pushing the federal government to resolve this issue and to get this addressed for people so they aren’t negatively impacted.”
Martin worries about how the federal government will handle the rush of exemption applications as tax time approaches. She expects many Alaska Natives and American Indians haven’t even thought about sending in the application yet. Evelyn Burdick, who was proactive and applied early in the process, says the nine month long wait for a response has been frustrating:
“I don’t want to be penalized for not having the healthcare.gov insurance. I’m trying to follow the rules and regulations that healthcare.gov set up and they’re not making it any easier.”
Late last month, Monique Martin was able to get Burdick’s exemption number for her from a contact at the federal government. Burdick is happy to have the number, but she still wants to see it in writing. She says she has no idea when it will arrive in her mailbox, but at this rate she’s not expecting it any time soon.
This story is part of a reporting partnership between APRN, NPR and Kaiser Health News.