Category: Health
Snohomish County medication “take back” locations
Submitted by Lori Hartelius M.S. LMHC MHP, Tulalip Family Services
What’s wrong with throwing my medicines in the garbage or flushing them down the toilet?
About 30 percent of medicines are not used. Flushing waste medicines pollutes the environment. Medicines are now found in our surface and ground water, as well as drinking water supplies. Wastewater treatment facilities do not remove most medicines. Throwing medicines in the garbage – especially controlled substances like OxyContin and other pain relievers – is not safe because the drugs can be found and used by others. Medicines thrown in the trash can also get into the environment. Leaving them in your medicine cabinets at home can also be dangerous and get into the wrong hands. Taking any unused medication to a “take back” location is easier than ever. There are numerous locations all around the county including most Bartell Drug stores and local police stations.
Stillaguamish Tribal Police 22714 6th Ave. NE, Arlington WA 98223 Mon-Fri, 8am – 10pm Accepts controlled substances 360-654-0645
Arlington Police Station 110 E. Third St., Arlington WA 98223-1300 Mon-Fri 9am-4pmAccepts controlled substances 360-403-3400
Bothell Police Department 18410 101st Ave. NE, Bothell WA 98011 Mon-Fri, 7am-4pm Accepts controlled substances 425-388-3199
Bartell Drugs, Bothell – Canyon Park 22833 Bothell-Everett Hwy , 98021 No controlled substances 425-485-3525
Brier Police Station 2901 228th St. SW, Brier WA 98036 Monday-Friday, 8:30am-4:30pm Accepts controlled substances 425-388-3199
Darrington Police 1115 Seeman St., Darrington WA 98241 Monday-Friday, 9:30am-12pm and 1:30pm-5pm Accepts controlled substances 425-388-3199
Bartell Drugs, Edmonds Pharmacy 23028 100th Ave. W, Edmonds WA 98020 Mon-Fri 9am-9pm; Sat 9am-6pm; Sun 10am-6pm No controlled substances425-774-4916
Edmonds Police 250 Fifth Ave. N, Edmonds WA 98020 Monday-Friday, 9am-4pm Accepts controlled substances425-388-3199
Snohomish County Sheriff – Jail 3025 Oakes Ave., Everett WA 98201 Monday-Friday, 8am-10pm Accepts controlled substances 425-388-3199
Bartell Drugs, Everett – Silver Lake 11020 19th Ave , Everett WA 98208 No controlled substances 425-379-5390
Bartell Drugs, Everett – Broadway 1825 Broadway, Everett WA 98201 No controlled substances. 425-303-2583
Bartell Drugs, Everett – Seattle Hill Road 5006 132nd Street SE Bldg. A, Everett WA No controlled substances 425-357-6129
Everett Police – North Precinct 3002 Wetmore Ave., Everett WA 98201 Monday-Friday, 8am-6pm Accepts controlled substances 425-257-8400
Everett Police – South Precinct 1121 SE Everett Mall Way, Everett WA 98208 Monday-Thursday, 10am-5pm Accepts controlled substances 425-388-3199
Group Health Cooperative, Everett Medical Center Pharmacy 2930 Maple St., Everett WA 98201 – Mon-Fri 8:30am-9pm; Sat 9am-3:30pm; Sun 9am-12:30pm No controlled substances 425-261-1560 425-388-3199
NCIS – Naval Station Everett 2000 W Marine View Dr., Bldg. 2000, Rm 234, Everett WA 98201 Accepts controlled substances 425-388-3199
Snohomish County Sheriff – Courthouse 4th Floor Courthouse; 3000 Rockefeller Ave., Everett WA 98201 Mon-Fri, 9:30am-4:30pm Accepts controlled substances 425-388-3199
Gold Bar Police 107 Fifth St., Gold Bar WA 98251 Monday-Friday, 10am-12pm & 1pm-4pm Accepts controlled substances 425-388-3199
Granite Falls Police 205 S Granite Ave., Granite Falls WA 98252 Monday-Friday, 9am-12pm & 1pm-5pm Accepts controlled substances 425-388-3199
Pharm-A-Save 207 E Stanley St #A, Granite Falls WA 98252 Monday-Friday 9am-7pm, Saturday 9am-6pm No controlled substances 360-691-7778
Bartell Drugs Frontier Village Pharmacy 621 SR9 NE, Lake Stevens WA 98258 Mon-Fri 8am-9pm; Sat 9am-6pm; Sun 10am-6pm No controlled substances 425-334-8410
Lake Stevens Police 2211 Grade Rd., Lake Stevens WA 98258 Monday-Friday, 8am-5pm Accepts controlled substances 425-388-3199
Bartell Drugs Lynnwood Pharmacy 17633 Highway 99, Lynnwood WA 98037 Mon-Fri 9am-9pm; Sat. 9am-6pm; Sun 10am-6pm No controlled substances 425-743-1136
Lynnwood Police 19321 44th Ave. W, Lynnwood WA 98036 Monday-Sunday, 8am-5pm Accepts controlled substances 425-388-3199
Marysville Police 1635 Grove St., Marysville WA 98270 Monday-Friday, 8am-3pm Accepts controlled substances 425-388-3199
Snohomish County Sheriff– North Precinct 15100 40th Ave. NE, Marysville WA 98271 Monday-Friday, 9am-4pm Accepts controlled substances 425-388-3199
Washington State Patrol – Marysville 2700 116th St. NE, Marysville WA 98271 Monday-Friday, 9am-12pm & 1pm-5pm Accepts controlled substances 425-388-3199
Bartell Drugs, Marysville 6602 64th St NE , Marysville WA 98270 No controlled substances 360-658-6218
Mill Creek Police15728 Main St., Mill Creek WA 98012 Monday-Friday, 9am-5pm Accepts controlled substances 425-388-3199
Snohomish County Sheriff– South Precinct 15928 Mill Creek Boulevard, Mill Creek WA 98012 – Monday-Friday, 10am-4pm Accepts controlled substances 425-388-3199
Monroe Police 818 W Main St., Monroe WA 98272 Monday-Friday, 8am-5pm Accepts controlled substances 425-388-3199
Mountlake Terrace Police 5906 232nd St. SW, Mountlake Terrace WA 98043 Monday-Friday, 8am-4pm Accepts controlled substances 425-388-3199
Bartell Drugs, Mountlake Terrace 22803 44th Ave W, Mountlake Terrace WA 98043 No controlled substances 425-771-3835
Mukilteo Police 10500 47th Pl. W, Mukilteo WA 98275 Monday-Friday, 9am-4pm Accepts controlled substances 425-388-3199
Snohomish Police 230 Maple Ave., Snohomish WA 98290 Monday-Friday, 10am-3pm Accepts controlled substances 425-388-3199
Bartell Drugs, Snohomish 1115 13th St, Snohomish WA 98290 No controlled substances 360-568-4153
Stanwood Police 8727 271st St. NW, Stanwood WA 98292 – NOTE: Stanwood Police Department medicine take-back location is temporarily closed from December 10 through March 10,2015 Accepts controlled substances425-388-3199
Bartell Drugs, Stanwood 7205 267th St NW, Stanwood WA 98292 No controlled substances 360-939-2188
Sultan Police 515 Main St., Sultan WA 98294 Mon-Thurs, 10am-12pm and 1pm-4pm Accepts controlled substances425-388-3199
Tulalip Healing: Understanding historical trauma in a Native context
By Kara Briggs Campbell, Special to Tulalip News
Pam James often says that she carries her grandmother’s pain.
“She was born in 1899 on theColville Reservation and she was taken away and put in a boarding school in eastern Montana,” James says as she begins a story familiar in her tribal family.
Her grandmother’s longing and loneliness were transmitted to James as a girl listening attentively to the family story. Researchers and counselors, like James, say trauma can be passed between generations in more than one way. Oral histories may be the most obvious way, but researchers say traumatic memories get recorded in our brains, and pass into cellular memory which we share from one generation with the next, and the next.
In the 1980s the terms historical trauma or intergenerational trauma were coined. This condition has been documented in groups that include the descendants of Holocaust survivors, descendants of survivors of Japanese Internment and of the Wounded Knee Massacre of 1890.
James, a counselor turned consultant who has taught groups about historical trauma for three decades, said historical trauma is a critical aspect of the American Indian experience today. It flares up when contemporary traumas trigger deeper known and unknown emotional wounds. It’s the extra weight of history that some people seem to carry in their psyches. It is a feeling of profound disempowerment.
“Historically, what have we learned after 500 years of cultural oppression? Through wars, epidemics, boarding schools, removal of children from families, removal of families from traditional lands, substance abuse, physical abuse, sexual abuse – we have become in many cases the oppressors. We see these things acted out today across Indian Country,” said James, who lives near the Skokomish Reservation. “We may not have the awareness of why, but we continue to pass the pain of our experiences from generation to generation.”
Shame, blame and an abiding sense of guilt are driving forces of historical trauma. Guilt for hidden things, even for half forgotten things, for things lost to memory and time.
Historical trauma manifests publically in tribal communities in ways that include family against family, a sense of who belongs and who doesn’t, who looks Indian, who doesn’t, James said. A tribal community may even be continuing such attitudes and practices without realizing or understanding that they come from the experiences of families and ancestors, some even in the colonial era long before we were born.
“A lot of those things impact ourselves and our children because of things that happened hundreds of years ago and that we keep passing from generation to generation. Without the realization, awareness or healing, we will self-destruct from within,” James said.
What does self-destruction look like? Overdoses, addiction, suicide, dropping out, tuning out, giving up. The impacts of historical trauma can go other ways too. They can manifest behaviorally as overachievers, control freaks or people who deny their emotions. For the most part survivors of historical trauma act out these behaviors without realizing that they may be tied to the experiences of their ancestors.
“In intergenerational trauma, each generation has an impact,” said Delores Subia BigFoot, who is director of the Indian Country Child Trauma Center at the University of Oklahoma Health Sciences Center. “Those that have been most impacted feel greater level of disempowerment as these layers of experience get added with each generation.”
James and BigFoot agree, Native people begin the healing process when they break the cycle of trauma through awareness. Or consider this: one generation can change the trajectory of a family or a whole tribal community. And in terms of the seventh generation, healing that begins today is very important.
Healing intergenerational trauma, as well as contemporary trauma, requires healing the whole person. Counseling and treatment work to a point. Deeper healing, James said, comes from reclaiming Native cultural identity and understanding traditional and family history. For James, the medicine wheel reminds us that healing the whole person includes spiritual, emotional, intellectual and physical.
“In our traditional ways of being we had cultural practices that brought us together to heal our wounds of the past and present,” James said. “Even when I was kid growing up we would come together and share stories of our family, our community, and our tribe telling our history and so forth. Everyone had their role in the community, grandmas and grandpas, aunties and uncles. We shared common family/community beliefs, values and experiences. You were learning your relationship to all things and your place in the world.”
Also within the oral histories of tribes – whether carried in words and written in our cellular memory in our bodies – there is a steady stream of health and resiliency that enabled tribal ancestors to survive their trauma.
“The reality is that the ancestors were resilient who survived to give you life,” James said. “The resiliency of who we are as a people speaks loudly to our ability to overcome trauma.”
What does it mean to be an Indian?
Pam James was working with tribal youth in the Puget Sound area when she asked a simple question: What makes you Indian?
“I was so surprised by the responses,” James said. “Some of them said, I don’t know. Others said because I was born here. Others said because I’m enrolled.”
“What I realized from those conversations is we aren’t teaching the young generations what makes them an Indian so they are conceptualizing what an Indian is in different ways than older generations do,” she said.
In terms of historical trauma, she wonders, are we teaching our youth those issues they need to understand to withstand the pressure?
So James researched and created the list below, which she shares when she presents at regional and national Native conferences about historical trauma. Her list is based upon the thinking of many tribal peoples and it reflects the traditional and cultural elements that make up a tribe or a village.
It may be a starting point for a conversation in a family or among friends.
What makes you an Indian?
Geographic Land Base – Living, Gathering, Hunting, Tools & Implements
Medicines and Foods – Plants, Animals, and the Preparation Process
Traditional Dress – Design, Creation, and Materials used
Common Language – Shared Dialect, Verbal, Body, Sign, Writings, Art
History and Stories – Creation, Oral/Visual Stories, Teachings, Roles & Responsibilities
Traditional Cultural Structure – Beliefs, Values, Ethics, Traditional & Legal Governance, Family, Relationships to All Things
Spiritual – Beliefs, Practice, Ceremonies, Songs, Music, Laughter
Being safe on social media
By Kara Briggs-Campbell, Special to Tulalip News
Social media is a player in every aspect of society these days.
Its profound impact hit home for the Tulalip Tribes after the tragic school shooting as an outpouring of grief, resentment and anger seemed to flow in every direction. Tulalip leaders called upon families to stop using social media all together in the weeks that followed, or at least not post in anger something that would be regretted later.
Off the reservation, law enforcement contacted those who posted hateful messages toward the tribe and its members, while regional and national news media scoured social media posts for information and photos of the victims.
Social media is an important form of communication for teens and adults. Increasingly, it is used in suicide prevention and education as way to directly inform teens and young adults, said Dr. Richard McKeon of Substance Abuse and Mental Health Services Administration.
“Social media is here to stay and it is up to those who use it to use it wisely,” he said.
Social channels are increasingly cooperating with organizations that seek to prevent everything from bullying to suicide.
In 2013, the National Suicide Prevention Lifeline announced its partnership with Facebook, which allows Lifeline to connect via an online chat with people who are posting suicidal ideas. Users can report suicidal posts by a friend on their news feed by clicking “mark as spam” then on the pop up screen choose, “violence or harmful behavior,” on the next pop up choose, “suicidal content.” Or enter your friends name or contact information.
U.S. Surgeon General Dr. Regina Benjamin, when announcing the partnership in 2011, said, “We must confront suicide and suicidal thoughts openly and honestly, and use every opportunity to make a difference by breaking the silence and suffering.”
Social media for many of us is more than just a tool. It is a way that we connect, stay in touch, entertain ourselves and share information.
Laura van Dernoot Lipsky, founder and director of the Trauma Stewardship Institute, said finding the people who are healthy for you to be around is the same on social media as it is in real life.
“People need pay very close attention to who they are spending time with,” she said. “It is a turning point in life when you can give thought to who you spend your time with.”
The same way someone in sobriety should avoid the old friends they used to drink and use with in person, they also need to avoid them online.
Social media can be beneficial for people who feel isolated and need to interrupt the isolation, she said. But if people are going online and reading negative stuff that is poison.
“The question is what do you take in? You can drink a lot of water and its good, or you can drink a lot of poison and it will kill you,” Lipsky said.
In a tribal community meeting last month with Dr. Robert Macy who is president of the International Trauma Center in Boston, tribal parents talked about the pressure that social media places on teens. Some talked about complex decisions to monitor teen’s online presence at the same time as respecting their privacy.
Macy said as long kids are dependent upon their parents to pay the rent and keep the lights on, parents have the responsibility to monitor everything that happens in their rooms or on their Facebook page or Twitter feed. For parents, the attitude must be, “I love you too much to let you hurt yourself.”
Macy had a warning for parents too.
Being too connected electronically can make you disconnected personally.
A 2014 study published in the Journal Academic Pediatrics found that mothers were regularly distracted at meal time by their smart phones. Overall, the study found that the use of cell phones and other devices during meals was tied with 20 percent fewer verbal interactions between mothers and their children, and 39 percent fewer nonverbal interactions. Those who had the highest use of mobile decides during meals were far less likely to provide encouragement to their children, researchers found.
So Macy urged the tribal families gathered to put their smart phones away during family time, and if you visit a friend, leave the phone at home or in the car. Then use the time to make a real person-to-person connection with someone you love.
Tips for students using social media
This list is based upon one published on the website of Carlton University in Canada. The tips are geared to college students, but apply as well to younger teens and for that matter to adults. The concern that Carlton University raises is that your social media posts will last forever on the World Wide Web. It is not overstating to say that this is new era in the history of the world. In past generations you could put your past behind you, you could move away, change your outlook. Now, if you have posted your life digitally on your social media sites, it will live online and be searchable by people in your future.
Privacy: Set all of your social networking accounts to private and maintain your privacy settings so you avoid posting too much personal information. On Facebook, don’t forget to set your privacy settings to include photos and videos that others post of you to avoid being found via basic Web searches.
Don’t over share: Don’t say anything you wouldn’t normally share with a prospective employer or your mother or your grandmother.
Stay offline when under the influence: If you’ve just spent a night partying with friends, keep your computer off, or your online mistakes could come back to haunt you. Sometimes referred to as “drunk Facebooking,” posting inappropriate comments or photographs while inebriated may cast a negative reflection on your online persona.
Stop Complaining: Avoid speaking negatively about school, current or previous jobs, family or friends. Similarly, don’t update your Facebook status only when you have something negative to say; find a balance so your digital persona doesn’t look too angry.
Separate social networking from job networking: Avoid using social networking sites like Facebook for professional or scholastic networking, and build up your career contacts on other sites like LinkedIn.com.
Generate positive content: Experts agree that the best way to counteract negative content is by generating positive information that will rank high on search engines like Google.
Where can I call for help?
To report an emergency dial 911
National Suicide Prevention Line: 1-800-273-TALK (8255)
Snohomish County Crisis Line: 1-800-584-3578
Crisis TEXT Line: Text “Listen” to 741-741
24 Hour Crisis Line: 1-866-427-4747
TEENLINK: 1-866-833-6546
Tulalip Tribes Behavioral Health Family Services: 360-716-4400
United Recovery Meeting, Jan 22
The Muckleshoot Tribe is spreading traditional food through schools

By Northwest Indian Fisheries Commission
The Muckleshoot Indian Tribe is making sure traditional foods are part of many of the meals it serves. Six kitchens across the tribe – including in schools and elder facilities – adopted new protocols to encourage the use of traditional foods.
The Muckleshoot Indian School is using the protocols to designate at least one day a week for traditional foods. The introduction of traditional food has been a learning process for both the kitchen staff at the school and the school community, said Shawn Saylor, the school kitchen coordinator.
The Muckleshoot school kitchen began introducing traditional foods soon after the protocols were in place four years ago. But even then, students were still able to choose a cold sandwich if they didn’t like the traditional option.
But after awhile that changed. “We don’t even make the sandwiches available on traditional food day anymore,” Saylor said. “The kids just forgot they didn’t like salmon. We don’t even do things like Sloppy Joe’s anymore because the kids just don’t like them.”
“Parents come in and visit us and they end up saying “I didn’t know they fed you so well here,’” Saylor said.
Each Thursday the kitchen staff prepares a meal following the traditional food protocols. Popular choices include halibut, seafood soup (which includes clams, shrimp, mussels and salmon), fish tacos or salmon. “We end up doing salmon a ton of different ways,” Saylor said. The school buys salmon directly from the tribe’s seafood enterprise.
The kitchen staff have also served elk and venison, even though it drives up the cost of the meals. “We will occasionally have a hunter donate meat to us,” he said.
The protocols also call for eliminating processed foods, trans-fat oils and high fructose corn syrup.
The kitchen staff also regularly meets with students to discuss how to make traditional Thursdays better. “We listen to the students and we like to explain why we do certain things in person,” Saylor said. “It builds trust between us and the kids. We even sometimes get food suggestions from them to try out.”
“The best part of my day is when kids come through the line on traditional food day and say “This is awesome,’” said Saylor.
Mainstream entities test the waters of ACA in Indian Country
By S.E. Ruckman, Native Times Special Contributor

OKLAHOMA CITY – Despite living in a state where Medicaid was not expanded, Oklahoma’s 38 federally recognized tribes have found a way to state tribal liaison, Sally Carter – and she has found her way to them. In this newly created position, Carter is quick to tell you that she considers Oklahoma to have 39 tribes because even though the Euchee are not federally recognized, they are state recognized. Breathlessly, she says she is learning fast.
“I still count them,” she said.
Carter carries Euchee concerns on health matters back to the state capital as part of a new stance where the health decision makers seek to repair a long and tenuous relationship between historical archetypes. When the Affordable Care Act (ACA) was passed in 2010, a series of listening sessions between Oklahoma and the tribes occurred at six different tribal jurisdictions across the state to talk about the federal health overhaul. Replete with opening ceremonies and songs, the state was figuratively stretching its hand toward its Native inhabitants.
From these beginnings, Carter takes the message back to the capital that the tribes want to be at the decision-making table with state leaders, including the newly re-elected Republican governor, Mary Fallin.
Carter said the tribes don’t just want to be told about important developments, they want to help shape the direction the state will take on things such as the implementation of the ACA and how to reduce health disparities like high smoking and diabetes rates in their nations.
To date, 1,638 American Indians in Oklahoma have enrolled for federal health insurance through ACA while 13,061 have enrolled nationally, according to a U.S. Department of Health and Human Services (HHS) report. When compared to the 9.1 million estimated Obamacare enrollees, American Indians number roughly 1 percent of all Americans who now have health insurance who had none before.
But that thing that makes Oklahoma’s Indian Country so different—that thing that separates it from other U.S. states with tribes – is that it has no official Indian reservations. A federal land allotment experiment from the 1900s crisscrossed the state’s territory into a veritable smorgasbord of jurisdictions – federal, tribal, municipal, state.
Carter is working on how to stimulate enrollment among Oklahoma tribes.
If the government wants to reach the American Indians here, it’s best to go to each tribe, Carter said. That was a go-to move state health officials embraced as they discussed ACA with the tribes. The things Carter found surprised her although she is an Oklahoma resident and had lived near various tribal jurisdictions for years.
“They are the only (minority) group that has to show their race,” she said, her voice lilting. “I mean, no other group has to do that. They have to prove it with an enrollment card of some kind.”
Official American Indian citizenship is important because the ACA has special provisions that allow Indians to “opt out” of having to enroll in federal health insurance, if they choose. But Indians need to fill out form OMB No. 0938-1190 that officially removes them, officials said. Not doing so will mean an eventual penalty.
“(ACA) is very complex and not one of us would say that we know it all,” Carter said. So the state took the best of what they knew after weeks of training on the health plan to several tribal jurisdictions. When all sides met, Carter said she was schooled. American Indians have strong opinions about the state/ federal government encroaching on their personal privacy and tribal sovereignty with this new federal health insurance.
Because Oklahoma chose not to expand Medicaid, enrolling American Indians in ACA takes a certain degree of cultural finesse and dogged persistence, Carter said. In other tribally populated states, like North Dakota, the move to expand Medicaid fills in where ACA may not be a strong priority, said Sen. Heidi Heitkamp, D-ND. The emphasis is reducing uninsured numbers, she said.
“The State of North Dakota expanded Medicaid, which has helped uninsured, low-income individuals and families, including many Native Americans throughout the state, get access to affordable health care,” Heitkamp said. “ Medicaid expansion is giving families opportunities they didn’t have before to afford to see a doctor regularly and get access to needed medications, while reducing costs for everyone – those with health coverage and those without.”
The Oklahoma tribal liaison added that even while enrollment curiosity abounded, many did not qualify for ACA because they did not file income tax returns. American Indians can enroll in ACA at any time – not just during enrollment periods, but their tax filings allow them also to file the exemption – if they chose to forgo coverage.
American Indians have a higher unemployment rate than other groups–peaking in 2013, according to the Bureau of Labor Statistics Current Population survey. Indian unemployment rates averaged 11.3 percent compared to 9.1 percent of the mainstream during that time. High unemployment rates among Indians tend to keep more Indians ineligible for ACA enrollment, Carter said.
What has also dampened Oklahoma’s outreach has been a distrustful relationship between the state and tribes—this makes it harder for federal initiatives to come through the front door, said Terry Cline, Oklahoma’s commissioner of health. He points to the good faith of the tribal/state meetings.
“I considered the listening sessions a good start,” he said. An official summary on the sessions reported 193 attendees at the six sessions, several of which Cline attended.
“We held those sessions to have open dialogue,” he said. “What you hear from one tribe might be different from another tribe says.”
As for ACA and tribes, a tribe’s type of relationship with the federal government, either Self-Governance or direct service, dictated outreach approaches because that’s how health dollars are administered by tribes in states, especially in Oklahoma, officials said.
Tribes that operate under provisions of the Indian Self Determination Act might outreach on ACA directly to members in their own tribally run health systems and tribes that are direct service entities may forgo outreach to their local Indian Health Service (IHS) service facility. In both regions, IHS and tribal facilities can accept ACA insurance from patients and lessen the amount of contract (out-of-IHS system) health dollars it spends, officials said.
“Tribes have a lot of interest in ACA,” Carter said. “Tribal leaders and the health department can inspire and direct tribal members to enroll.”
Both of the tribal-to-federal relationships are considered when the state of Oklahoma contacts tribes, and the state tends to follow the federal approach, Carter said. Putting on different hats to deal with different tribes is prudent.
“Tribes need to see people they know and that they can trust who know about American Indian provisions,” she said. “I believe in face-to-face interactions. States usually contact them (tribes) with emails or letters, but a relationship needs to be worked on and allowed to develop.”
Cline said no special state appropriations exist to outreach to tribes for ACA enrollment in Oklahoma but he’s optimistic that other types of federal grants to reduce health disparities will help. The health commissioner said he knows Oklahoma has room for ACA Native growth through grants.
The HHS report points out that Oklahoma has the highest density of Indians among Federally Facilitated Marketplace (FFM) states with 3.5 percent of the population followed by Wyoming, with 3.1 percent. Wyoming’s total Native ACA enrollment stands at 309, the report shows.
At this point, Oklahoma seems to lead the state in the number of Natives it has enrolled, just exceeding figures for California. But as enrollment rolls on, officials expect more American Indians to register. Indian Country (the term used to characterize where a federal-tribal relationship exists) extends beyond Oklahoma.
Other states with significant Native populations include Arizona, California, New Mexico, South Dakota and North Dakota. ACA data gathering for Native numbers is in its infancy, organizers said. They say the goal is to pool their information from various regions (via Indian advocacy agencies) to get a more precise picture of Native ACA enrollment. Due to their smaller population numbers, American Indian statistics are often overlooked, officials said.
Other mainstream entities who track the progress are unclear about just how many have actually signed up for ACA. Michelle McEvoy, vice-president of survey, research and evaluation for the Commonwealth Fund, said that no Native specific information has been garnered by her group.
“Latinos currently represent about 17 percent of the U.S. population, so they have a greater probability of being sampled than American Indians who represent about 1.2 percent of the U.S. population,” she said.
Likewise, the non-profit Enroll America, relies on Native ACA enrollment numbers from federal sources, wrote Jessica McCarron, deputy press secretary, by e-mail.
“We do work with partners at the local level to reach different communities, like Native American groups in certain parts of the country,” McCarron stated. “We work with a few partners who have made outreach to tribal communities a high priority.”
Meanwhile, Carter is optimistic about ACA enrollment and reaching American Indians in Oklahoma.
“(ACA) is bigger than all of us,” she said. “We can’t do this alone; it only happens when the state extends its hands across the table and says we need to do this for all the people.”
– This story was funded by the University of Southern California’s (USC) Annenberg School of Journalism as one project undertaken by the 2014 class of California Endowment Health Journalism Fellows. S.E. Ruckman is writing a three-part series on the Affordable Care Act (ACA) in Indian country. In addition to mainstream viewpoints, American Indian health advocates and American Indian enrollees are visited to gauge the national health plan’s implementation in Native populations. Fellows’ projects can be found at www.reportingonhealth.org.
NATIVE AMERICAN ACA ENROLLEES STATE ENROLLMENT TOTALS
*Wyoming: 309
*New Mexico: 566
*Oklahoma: 1,635
+California: 1,401
*Arizona: 514
*North Dakota: 82
*South Dakota: 271
TOTAL: 13,061
Sources: (March 2014) *HHS Summary Report; +California Department of Health Care Services
Tulalip Stop Smoking Program can help you reach your goals
Why becoming a quitter can make you a winner
By Brandi N. Montreuil, Tulalip News
The discussion to quit smoking cigarettes can be as stressful as trying to quit. The nagging. The pressure to succeed. The feeling of failure. The cost. The nagging. The fear. The withdrawals. The pressure. The nagging. Does this sound similar? Are you feeling like you need a smoke break as you read this? If so, then I know exactly how you feel and so does 42.1 million other people in the U.S. who smoke everyday.
I started smoking when I was 20-years-old, because it made me feel cool. Cliché as it is, it was my reason to commit to buying my first few packs and getting past the sick feeling I got every time I tried to inhale. Eventually I got over the sick feeling and I developed a habit.
Cigarettes contain 600 ingredients with nicotine as the key ingredient, giving it that addictive component. When smoked, a cigarette creates over 4,000 harmful chemicals including arsenic, commonly used in rat poison, formaldehyde, which is used as an embalming fluid, naphthalene, an ingredient found in moth balls, and tar, a material used to pave roads and to seal roofs.
According to the Centers for Disease and Control, Americans spent $8.4 billion on tobacco in 2011, and cigarette smoking is the number one leading cause of preventable death in the United States, “accounting for more than 480,000 deaths, or one of every five deaths, each year.”
My decision to quit smoking for good came in the beginning of 2014. I had tried, unsuccessfully to quit the previous year, but in 2014 I got the gusto to commit to quitting after meeting with the cessation specialist Ashley Tiedeman with the Tulalip Stop

Smoking Program. Now I have been smoke free for a year.
The Tulalip Tribes Stop Smoking program provides an essential lifeline for those trying to quit in the Snohomish County. Through the program you will receive one-on-one help tailored to your needs, free of cost. The program provides support and cessation supplies such as the popular nicotine patches and gum that help smokers kick the habit.
There were multiple factors that led to my decision to quit, which included the financial burden of smoking. I spent roughly $1,296.36 in 2013 on packs of Marlboros. The toll on my health was starting to be felt outwardly. I had decreased oxygen levels leading to shortness of breath. My teeth were yellowing and I experienced withdrawal symptoms when I couldn’t smoke, which include irritability, hunger, coughing, dry mouth, tiredness or drowsiness, and trouble sleeping.
When meeting with Tiedeman, I learned there were a variety of options available to me in my journey to quit the habit. The most common option smokers consider is the “cold turkey” method, which involves literally ceasing to smoke a cigarette, despite the withdrawal symptoms you experience. This is the method that I used to quit. Other methods include herbal remedies and medication to help tackle cravings, the number one obstacle people face when trying to quit.
The other obstacle smokers face trying to quit is fear of failure, which is why a majority of smokers try to hide their attempts at quitting. Routines developed as a smoker, such as pairing the activity of smoking with another daily activity like driving or after eating, also makes it difficult to quit.
To help participants, the Stop Smoking program helps smokers create a toolbox of resources to draw from when they experience temptations and cravings.
“There is no pressure. We help people develop coping skills to get past smoking. We meet with them on a weekly basis to help them stay on track, and help them assess where they succeeding and having difficulties, then develop action plans for them. There is no time limit to quitting. It is just day by day,” said Tiedeman.
For help quitting smoking or more information on the program, please contact Ashley Tiedeman at 360-716-5719.
Brandi N. Montreuil: 360-913-5402; bmontreuil@tulalipnews.com
Mom’s death inspires advocacy for those living with addiction

Rico Jones-Fernandez waits in a gravel lot outside a vacant building on the Tulalip Reservation on Tuesday for anyone wishing to exchange needles.
By Andrew Gobin, The Herald
TULALIP — Since his mother’s death four years ago from a drug overdose, Rico Jones- Fernandez has worked to save other lives that might be lost.
His focus has been on people living with addiction on the Tulalip Indian Reservation.
“I have the ability to do something, so it is my responsibility to do something,” he said.
Jones, a member of the Tulalip Tribes, has been an advocate for expanding outreach programs on the reservation, particularly efforts that reach people who are not yet ready for rehabilitation.
Last year, Jones worked to develop a law that shields addicts from arrest and prosecution of misdemeanor offenses when they are seeking medical assistance to save a life. In recent months, Jones also has played a key role in bringing a syringe exchange to the Tulalip community, the first program of its kind for the reservation.
In 2010, Jones’ mother, Lois Luella Jones, died of a drug overdose. Her friends did nothing to help her, fearing they themselves would be arrested.
His mother’s story inspired Jones to draft a 911 Good Samaritan law for the Tulalip Tribes in hopes that others might be saved.
In June, the Tulalip Tribal Council passed the Lois Luella Jones Law, which provides temporary immunity from prosecution for low-level offenses if the person is attempting to get medical attention for themselves or somebody else in any emergency.
A higher value is placed on saving lives than filing misdemeanor drug charges, Jones said.
In May of last year, Tulalip Prosecutor Dave Wall told Tulalip News, “In terms of the war on drugs, when someone is overdosing, the war has been lost. The battle for that person’s life is now the focus.”
Jones began volunteering with the Snohomish County Syringe Exchange in 2014 to learn how he might start a similar program on the reservation. The exchange offered to expand their service and two months ago began exchanging needles at Tulalip every Tuesday.
The goal is not to enable drug use, but to prevent the spread of disease.
“Hepatitis-C and HIV get on everything, not just syringes. We exchange everything. The cooker, the cottons and the tourniquets,” Jones said.
Some criticize syringe exchanges, concerned these types of programs are giving needles away, fueling a problem.
“People already have needles that they are using, and reusing,” Jones said. “This isn’t about giving them needles, it’s about making sure they have a place to safely dispose of dirty needles in exchange for clean, safe syringes.”
His mother’s death continues to drive him, but it is the promise of the future that fuels Jones’ perseverance.
“I get tired. I face a lot of opposition when I try to bring programs like this to our community,” Jones said. “But I made a promise to myself and my son that this would be a safer place for him. I can’t give up.”
Currently, Jones is seeking approval from the tribal council to increase access to Naloxone on the reservation. If approved, people would be trained to administer Narcan, a compound that counters the effects of a drug overdose.
Jones, who has never been an addict, hopes to spare others the sorrow of loss he knows too well.
“It’s not about drugs or enabling people; it’s about people’s lives. All I do is in hopes of saving lives,” he said.
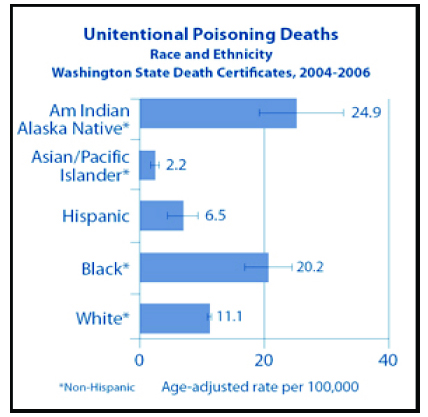
In 2013, 580 people died in Washington from opioid drug overdoses, 86 of whom were from Snohomish County, and Providence Regional Medical Center Everett reportedly treated 440 cases of opiate poisonings.
Grounding Yourself in Uncertain Times
Do you have things that are weighing you down from last year, the year before, the years before that?
There is a new group at Tulalip to help you work through some of those issues, perhaps some grief, frustration, confusion, all the feelings one has when things happen in life that leave you off center.
This is a drop in group, open to the Tribal Community